About Brachytherapy
Radiotherapy can be divided into external beam radiotherapy (EBRT) and brachytherapy; depending on whether the radiation source is external to the patient (EBRT) or internal/in close proximity to the patient (brachytherapy) 1.
The word ‘brachy’ is Greek for ‘short-distance’, and it is the short distance between the radiation source and the tumor which enables brachytherapy to offer highly precise radiotherapy. This way it is possible to safely deliver high doses of radiation within a short period of time to eliminate and shrink tumors.
First practiced over 100 years ago, modern brachytherapy utilizes a combination of state-of-the-art imaging, computer-based planning and treatment delivery technologies to deliver optimal radiotherapy.
Which cancers can be treated with brachytherapy?
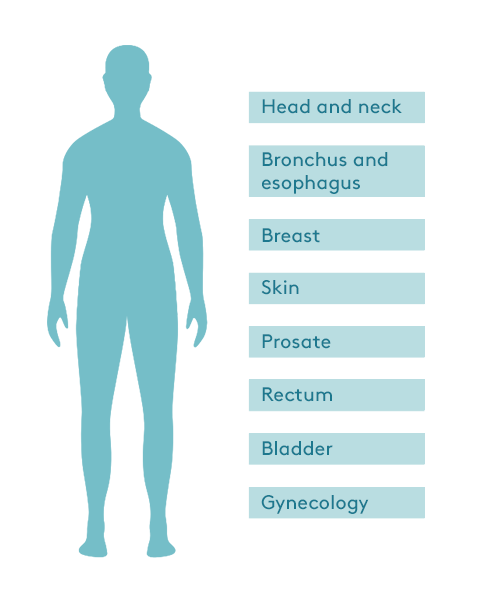
Brachytherapy is at the forefront of cancer treatment and addition of brachytherapy to cancer treatment has resulted in excellent patient outcomes 2-5. It is most commonly used in the treatment of cervical cancer, prostate cancer, breast cancer and skin cancer, but is also successfully used for cancers of many other body sites 6,7.
Brachytherapy allows an optimal dose and distribution of radiation to be calculated for each individual patient. This radiation dose can be delivered directly to the tumor site precisely, efficiently and safely, providing cancer cure rates comparable to surgery and EBRT for many types of cancers 8 -10. The precision of brachytherapy minimizes the exposure of surrounding healthy tissues to unnecessary radiation. In many cases, brachytherapy is combined with external-beam radiation therapy to get the best results 7, 11.
Brachytherapy also enables higher radiation doses to be given safely in a shorter period of time. A course of brachytherapy can typically be completed in 1 to 5 sessions, compared to daily treatments for many weeks with conventional EBRT 12. Brachytherapy is therefore more time efficient and patient friendly, allowing patients to get back to their everyday life sooner.
References
- World Health Organization. Available at: https://apps.who.int/iris/bitstream/handle/10665/339912/9789240019980-eng.pdf. Accessed 02 November 2021.
- Pötter, R., Tanderup, K., Schmid, M. P., Jürgenliemk-Schulz, I., Haie-Meder, C., Fokdal, L. U., … & Yoshida, K. (2021). MRI-guided adaptive brachytherapy in locally advanced cervical cancer (EMBRACE-I): a multicentre prospective cohort study. The Lancet Oncology, 22(4), 538-547.
- Hoskin, P. J., Rojas, A. M., Ostler, P. J., Bryant, & L. Lowe, G. J. (2021). Randomised trial of external-beam radiotherapy alone or with high-dose-rate brachytherapy for prostate cancer: Mature 12-year results. Radiotherapy and Oncology, 154, 214-219.
- Khan, A. J., Chen, P. Y., Yashar, C., Poppe, M. M., Li, L., Abou Yehia, Z., … & Kuske, R. (2019). Three-fraction accelerated partial breast irradiation (APBI) delivered with brachytherapy applicators is feasible and safe: First results from the TRIUMPH-T trial. International Journal of Radiation Oncology* Biology* Physics, 104(1), 67-74.
- Pellizzon, A. C. A., Fogaroli, R., Chen, M. J., Maia, P., Gondim, G., de Castro Guedes, D., … & Silva, M. L. G. (2020). High-dose-rate brachytherapy using Leipzig applicators for non-melanoma localized skin cancer. Journal of contemporary brachytherapy, 12(5), 435.
- Skowronek, J. (2017). Current status of brachytherapy in cancer treatment–short overview. Journal of contemporary brachytherapy, 9(6), 581.
- Chargari, C., Deutsch, E., Blanchard, P., Gouy, S., Martelli, H., Guérin, F., … & Haie‐Meder, C. (2019). Brachytherapy: An overview for clinicians. CA: a cancer journal for clinicians, 69(5), 386-401.
- Guo, X. X., Xia, H. R., Hou, H. M., Liu, M., & Wang, J. Y. (2021). Comparison of Oncological Outcomes Between Radical Prostatectomy and Radiotherapy by Type of Radiotherapy in Elderly Prostate Cancer Patients. Frontiers in Oncology, 11.
- Lee, C. T., Lehrer, E. J., Aphale, A., Lango, M., Galloway, T. J., & Zaorsky, N. G. (2019). Surgical excision, Mohs micrographic surgery, external‐beam radiotherapy, or brachytherapy for indolent skin cancer: An international meta‐analysis of 58 studies with 21,000 patients. Cancer, 125(20), 3582-3594.
- Hepel, J. T., & Wazer, D. E. (2020). Partial Breast Irradiation Is the Preferred Standard of Care for a Majority of Women With Early‐Stage Breast Cancer. Journal of Clinical Oncology, 38(20), 2268-2272.
- Gupta, S., Maheshwari, A., Parab, P., Mahantshetty, U., Hawaldar, R., Sastri, S., … & Badwe, R. (2018). Neoadjuvant chemotherapy followed by radical surgery versus concomitant chemotherapy and radiotherapy in patients with stage IB2, IIA, or IIB squamous cervical cancer: a randomized controlled trial. Journal of Clinical Oncology, 36(16), 1548-1555.
- Royal college of radiologists publication, available at: https://www.rcr.ac.uk/system/files/publication/field_publication_files/brfo193_radiotherapy_dose_fractionation_third-edition.pdf Accessed 03 November 2021.
